
The small night’s rubric
Here is now a basic part of ultrasound: venous investigation, and a setting slightly different than ours usual: medical transportation. Anyway, this case can be extrapolated to any setting.
Initiating a medical transportation, we take in charge a 19 year old female, at the 7th day of a toxic shock syndrome. There was initially severe ARDS, circulatory failure, renal, hematologic and cutaneous troubles. The cutaneous disorders indicate management in a specialized unit, and the transportation is decided once the vital lesions stabilized.
At the bedside, we make our routine ultrasound, as we do for any critically ill patient [1], using our ultraportable Tringa S-50 (Pie Medical, 1,850 kg, 2200 cc, analogic resolution). This protocol includes basic points that can interfere with the safety of the transportation: pneumothorax, interstitial edema, main stem intubation, left ventricle systolic failure, deep venous thrombosis (Figure 1 & 2), hemoperitoneum especially. These simple checkings require less than 2 minutes for a trained user, when all is clear*.
At the 20th second of the analysis, our routine scanning detects a patent, floating venous thrombosis (Fig. 3), occupying a large part of the inferior vena cava, with a cross sectional area of 50%. A femoral venous catheterization is the supposed source.
The examination is interrupted, since there is evidence for major risk of the transportation - we must consider that this thrombosis will support all mechanical forces of the moving on the stretcher, the ambulance, the vibrations of the airplane (propeller action, taking-off or landing...). After collegial talks, once evaluated the risk/benefits, the transportation is temporarily postponed, till this acute problem is solved.
The patient had, two days before, a transient episode of respiratory wsorsening, that required changes in the ventilatory parameters (PEEP adaptation). It can be assumed that this was - possibly - a first episode of pulmonary embolism. These unexplained episodes are routine in the ICU (routine does not mean unsignificant). Seeing by ourselves the high rate of venous thrombosis (after central venous catheters) in the ICU, we postulate that pulmonary embolism occupies a larger place than usually considered.
We also think, retrospectively, to all these stories of sudden cardiac arrest (or circulatory failure) that physicians transporting critically ill patients have known, and often labelled acute decompensation of hypovolemia. Ultrasound provides a direct visualization of the critically ill.
* Average time for experienced users:
Lung sliding : two seconds x 2
diffuse B lines on four areas : one second x 4
LV contractility: time for 2 or 3 systoles (variable with heart frequency, usually 3 seconds)
Hemoperitoneum: 20 seconds for scanning the whole abdomen
Venous thrombosis:
Inferior vena cava: 10 seconds if favorable body habitus
Iliac veins: 15 seconds x 2
Common femoral veins: 5 seconds x 2
Our coupling system, that allows bypassing the current gel, uses a product (under commercialisation) over a compress. In addition to the comfort of the patient (and operator), it allows massive gain of time in such whole-body investigations.
Figures
Figure 1

Basic technique, normal aspect. We privilegiate anterior, transversal approach. This approach allows immediate location of the vein, which is anterior to the rachis, at the right of the aorta (A). In the case of gas interposition, a mild compression using the free hand allows pulling the gas away. A microconvex probe use greatly facilitates this maneuver (difficult with an abdominal one). Arrows, inferior vena cava. V: left renal vein - this is the landmark we use since long for measuring IVC caliper [2].
Figure 2
Complete thrombosis of the inferior vena cava. Tissue-like mass at the exact level of the IVC. A scanning to the top and bottom indicates the tubular nature of this image, thus ruling out pitfalls (adenomegaly compressing the IVC may mimick this static pattern).
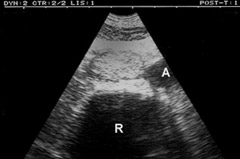
Figure 3

Demonstration of the floating character of a thrombosis (M) on a static image, by using the M mode: sinusoidal movements (arrows) indicating instability of the thrombosis.
Références
1. Lichtenstein D & Axler O (1993). Intensive use of general ultrasound in the intensive care unit, a prospective study of 150 consecutive patients. Intensive Care Med 19:353-355
2. Lichtenstein D & Jardin F (1994). Appréciation non invasive de la pression veineuse centrale par la mesure échographique du calibre de la veine cave inférieure en réanimation. Réanimation Urgences 3 (2), 79-82
NB : This application is detailed in “General ultrasound in the critically ill” , published by Springer-Verlag (recently reprinted).